High-Quality Surfactants for Global Markets - Trusted Manufacturer
Surfactant Superhero: Rescuing Tiny Lungs One Dose at a Time
(how to administer surfactant)
Breathing. It’s automatic for most of us. But for fragile newborns, especially those arriving too soon, that first breath can be a monumental struggle. The hero in this critical moment isn’t wearing a cape. It’s surfactant. This blog dives into the vital world of surfactant administration, the life-saving technique giving premature babies the precious gift of easier breaths.
1. What Exactly is Surfactant? Liquid Gold for Lungs
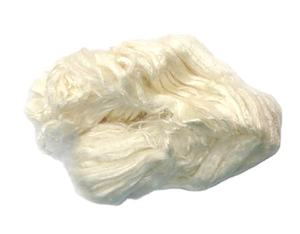
Think of surfactant as nature’s miracle soap for the lungs. It’s a complex mix of fats and proteins. Our bodies make it naturally. Its job is crucial inside the tiny air sacs (alveoli) where oxygen enters our blood. Surfactant coats these sacs. It dramatically lowers surface tension. Surface tension is the force making water form droplets. Inside the lungs, high surface tension makes the air sacs collapse after every breath out. This makes breathing incredibly hard work.
Premature babies often lack enough surfactant. Their lungs are simply underdeveloped. Without enough surfactant, their air sacs stick together. Each breath becomes a huge effort. This condition is Respiratory Distress Syndrome (RDS). RDS is a major threat to premature infants. Surfactant replacement therapy steps in here. Doctors give the baby artificial or natural surfactant. This replaces what the baby’s lungs are missing. It’s like adding soap to water – suddenly, things flow much easier.
2. Why Do Premature Babies Desperately Need Surfactant? The Fight for Air
The need is urgent and simple: survival. Premature lungs are delicate structures. They haven’t had enough time to mature. Producing adequate surfactant is one of the last things to develop fully. A baby born before 34 weeks is very likely to be surfactant-deficient. The consequences are severe.
Without surfactant, the air sacs collapse constantly. The baby must use immense effort just to reinflate them with each breath. This leads to rapid, labored breathing. The baby might grunt, flare their nostrils, or see their chest sink in with each breath (retractions). Oxygen levels drop. Carbon dioxide builds up. The baby tires quickly. Exhaustion sets in. Without intervention, respiratory failure happens. Heart strain follows. Organ damage becomes a real risk.
Surfactant administration tackles RDS head-on. It directly addresses the root cause – the missing soap-like substance. Giving surfactant quickly improves lung function. It makes breathing easier immediately. Oxygen levels rise. The baby conserves vital energy. This reduces complications like lung injury from ventilators. It significantly cuts the risk of death from RDS. For these tiny patients, surfactant isn’t just medicine; it’s often the difference between life and death.
3. How is Surfactant Given? A Delicate Delivery
Administering surfactant is a precise procedure done by skilled medical professionals, usually neonatologists or experienced neonatal nurses. Speed and accuracy are key. It’s typically done right in the Neonatal Intensive Care Unit (NICU). Here’s the common approach:
First, the baby needs stable access to the airway. This usually means the baby is intubated. A breathing tube is placed gently down the windpipe (trachea). The tube connects to a ventilator. The ventilator helps the baby breathe during the procedure.
The surfactant itself comes in a small vial. It’s a milky-white liquid. The medical team warms it slightly. Cold surfactant could shock the tiny lungs. They draw the exact dose into a syringe. The dose is based strictly on the baby’s weight.
The doctor carefully inserts a thin, soft catheter through the breathing tube. They guide the catheter down into the trachea. The tip of the catheter needs to be positioned just right. Then, the surfactant is slowly injected. The injection happens in small amounts. The doctor might turn the baby slightly side-to-side. This helps the surfactant spread evenly into both lungs.
The breathing tube stays connected to the ventilator. The ventilator provides breaths while the surfactant works. The team watches the baby’s vital signs closely. Oxygen levels, heart rate, and breathing effort are monitored constantly. They watch for any changes. Sometimes, babies need extra support right after the dose. The surfactant starts working fast. Improvements in breathing and oxygen levels are often seen within minutes or hours.
4. Surfactant Applications: Beyond the Tiniest Babies
While surfactant therapy is synonymous with saving premature infants with RDS, its uses extend further. Understanding surfactant helps manage other conditions too.
The primary application remains clear: treating and preventing RDS in premature newborns. It’s standard care worldwide. Doctors often give it preventively to very premature babies right after birth. They might give it as rescue treatment if RDS develops later. Research keeps refining the best timing and dosing strategies.
Surfactant research explores other areas. Scientists study its role in conditions like Acute Respiratory Distress Syndrome (ARDS) in older children and adults. ARDS involves severe lung inflammation and surfactant dysfunction. Giving surfactant might help in some cases. Results are still under investigation. Surfactant is also used experimentally in cases of near-drowning. Lung damage from inhaled water can wash away natural surfactant.
Surfactant science has broader impacts too. Understanding how it works inspires things like better drug delivery systems. It helps develop improved artificial lungs. Surfactants are key in many industrial products. Firefighting foam relies on surfactant principles. Detergents and dish soaps use surfactants to break down grease. The study of lung surfactant teaches us valuable lessons about surface chemistry.
5. Surfactant FAQs: Answering Common Questions
Parents and caregivers naturally have questions about this critical treatment. Here are some frequent ones:
Is surfactant safe? Yes, surfactant therapy is very safe overall. The benefits far outweigh the risks. Potential side effects are usually minor and temporary. They might include brief drops in oxygen or blood pressure during administration. These are managed easily by the NICU team. Long-term side effects are rare.
Where does the surfactant medicine come from? There are two main types. Natural surfactants are extracted from animal lungs (usually cows or pigs). They closely mimic human surfactant. Synthetic surfactants are made in labs. They contain key synthetic fats and proteins. Both types are effective. Doctors choose based on availability and specific needs.
How long does it take to work? The effects are often rapid. Many babies show better lung expansion and oxygen levels within minutes. The full benefit usually peaks within a few hours. The baby might need less ventilator support soon after. The improvement can be dramatic.
Can a baby get surfactant more than once? Yes, sometimes babies need a second dose. This happens if the first dose doesn’t achieve the needed improvement. It might happen if the baby’s condition worsens again later. Doctors decide based on the baby’s breathing and oxygen needs.
(how to administer surfactant)
How is surfactant stored? Surfactant is stored refrigerated before use. It’s kept in a controlled environment. The medical team warms it gently just before giving it. This ensures it’s at the right temperature for the baby’s delicate lungs. Proper storage maintains its effectiveness.